Navigating Service Canada’s Benefits: Discover Your Options
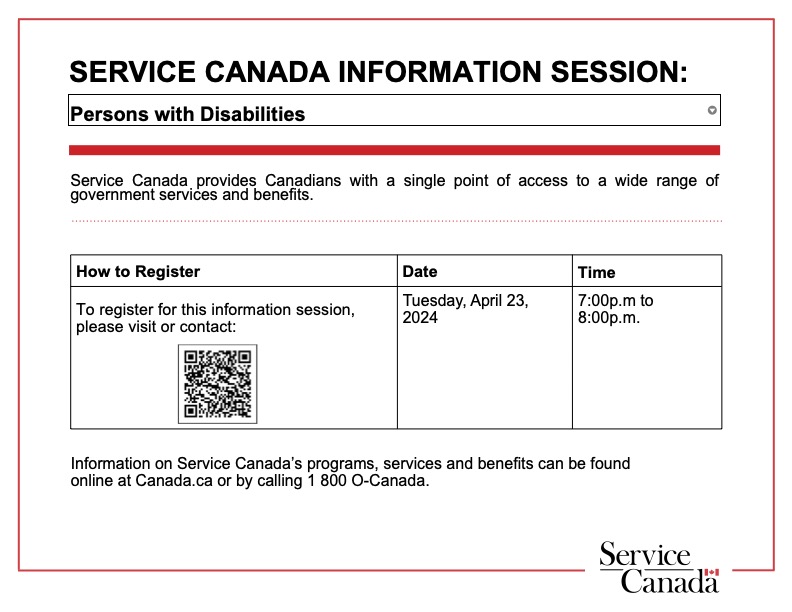
Curious about federal government benefits? Unsure of what’s accessible to you and how to navigate the application process? Join us on April 23rd for an enlightening session with Acting Citizen Services Specialist, Vanessa Gaspar, as she outlines the array of benefits provided by Service Canada.
COVERING:
Employment Insurance Benefits (EI)
Sickness Benefits
Compassionate Care Benefits
Caregiving Benefits for children and adults
Canada Pension Plan Disability Benefit (CPP-D) Including CPP Children’s Benefit
Canadian Dental Care Plan (CDCP)
Opportunities Fund for Persons with Disabilities (OF)
Skills Training and Employment Supports
This webinar will not be recorded. Please try to attend the LIVE webinar. Resources will be posted to our website following the webinar.
Lupus Ontario AGM
Learn about Type 1 or Type 2 Lupus with Dr, Murray Urowitz, who presented this lecture at this year’s AGM.
Pregnancy in lupus and fertility management
This session will delve into the intricate challenges faced by women with lupus during pregnancy and the effective management of fertility issues. Medication considerations will also be addressed in this comprehensive discussion.
About Dr. Carl Laskin: Dr. Carl Laskin, a prominent figure at the University of Toronto since 1983, brings over 30 years of expertise to our webinar. Currently serving as the Managing Director of TRIO Fertility in Toronto, Dr. Laskin is a distinguished specialist in rheumatology, obstetrics & gynecology, and reproductive endocrinology. Dr. Laskin has been actively involved in groundbreaking clinical research, particularly in areas such as recurrent miscarriage and reproductive medicine in individuals with rheumatic diseases. As a past president of the Canadian Fertility & Andrology Society, Dr. Laskin holds a unique position at the intersection of rheumatology and fertility.
Unlocking the Power of Biologics: A Webinar with Dr. Tselios
“Unlocking the Power of Biologics: A Webinar with Dr. Tselios” was an informative online event where Dr. Tselios, an expert in the field of biologics, shared insights into the potential of biopharmaceuticals. During the webinar, Dr. Tselios discussed the revolutionary impact of biologics in healthcare, highlighting their applications in treating various diseases.
CARE for All – Symposium 2023 Playlist
The Lupus Ontario Virtual Symposium was on October 21st beginning at 10 a.m., with presentations by medical professionals covering new research and innovative ideas. This year’s theme was “CARE 4 All” with topics covering Community, Access, Resources and Education.
Transition of Care – from Paediatric to Adult
We are honoured to have Dr. Stephanie Wong, our esteemed Lupus Ontario Geoff Carr Fellow from SickKids Hospital. Dr. Wong will share her expertise on the transition of care and medication for children and youth as they move from paediatric care to adult care. The webinar will also include a discussion with a young adult who has recently transitioned to adult care.
Why Early Access is Important To Prevent Organ Damage
The informative and engaging webinar with Dr. Zahi Touma discussing the critical importance of early access to medical care to prevent organ damage in patients with chronic diseases took place on May 18th, 2022, from 7:00-8:00 PM. Dr. Touma, a renowned Rheumatologist and Clinician-Scientist with extensive expertise in the management of autoimmune diseases, such as lupus and vasculitis, shared valuable insights during the event. The webinar provided an overview of the different types of organ damage that can occur in patients with chronic diseases and explained how early detection and timely intervention can significantly improve patient outcomes. Dr. Touma also addressed the challenges faced by patients and healthcare providers in accessing care and provided practical tips on overcoming these barriers.
This recorded webinar is now available for viewing. It is a must-watch for healthcare providers, patients, and caregivers who want to gain knowledge about the importance of early access to medical care and stay updated with the latest advances in the management of chronic diseases. Don’t miss the opportunity to hear from one of the leading experts in the field and have your questions answered in real-time.
Symposium Playlist
October 22nd 10 AM – 2:30 PM EST
Additional Information About Lupus
Articles
Canada’s COVID Immunization Plan
Communicating with Your Health Care Professionals
COVID-19 Vaccination Recommendations for Special Populations – Ministry of Health
COVID-19 Vaccine Third Dose Recommendations – Ministry of Health
Eye Health and Eye Care at Home
Government Supports – Caregiving Benefits
Government Supports – Trillium Drug Program
LED Lighting and Photosensitivity
Lupus Checklist by GlaxoSmithKline
Mental Health Commission of Canada’s Mini Guide to Help Employees’ Mental Health Through Winter
POA – Power of Attorney for Personal Care
Red Blood Cell Alterations Contribute to Lupus
2020-2021 Influenza Vaccine for Lupus Patients
Diet + Nutrition
Lupus in the News
Brian Crombie Radio Hour – Epi 392 – Lupus Awareness Month with Rupinder Sandhu
Canada Now – Jeff Sammut with Brynn Clark
Charitable Choices: Lupus Ontario, Awareness and Support For Canadians – Toronto Guardian
Presentations + Handouts
What the gut got to do with it PDF
Raynaud’s Association of America PDF
Sjogrens Society of Canada PDF
Fighting Fatigue: Using Energy Management Strategies
ADP- Assistive Devices Program
Common Rashes and Skin Infections Seen in Systemic Lupus Erythematosus (SLE)
Dealing with Summer UV, Heat and Humidity
Gut Health: It’s Not the Food’s Fault Presentation
Lupus and Co-Existing Fibromyalgia
Makeup, Skin Care & Getting Ready for Summer Webinar Presentation
Managing Your Life with Lupus Webinar Presentation
Nutrition During a Pandemic Webinar Notes
Pharmaceutical and Government Programs to Help Pay for Medications
Plaquenil (Hydroxychloroquine): Eye Safety, Testing and Dosage
Practical Strategies for Managing Stress and Anxiety Presentation
SLE and COVID-19: What is the Evidence?
Taking Care of Our Mental Health During Social Distancing
Therapeutic Laser for Symptom Management
Treatment and Support Teams Worksheet
The Story Behind Cognitive Impairment and Lupus Brain Fog Presentation
Recordings
Webinar Q&A with Dr. Touma and Dr. Barraclough
Lupus Education
No one knows for sure what causes lupus. What we do know is that the immune system (the body’s defense against viruses and bacteria) is not able to tell the difference between intruders and the body’s tissues. The immune system attacks parts of the body, which causes inflammation and creates the symptoms of lupus. Lupus is not contagious and is not related to AIDS or cancer. It belongs in the family of diseases that includes rheumatoid arthritis, multiple sclerosis, juvenile diabetes, and scleroderma.
Lupus is a chronic disease caused by inflammation in one or more parts of the body. The majority of people diagnosed with lupus are women in the prime years of their lives – between the ages of 15 and 45 years. Especially impacted are communities that include women of African, Caribbean, Asian, and Aboriginal descent.
In an autoimmune disorder the immune system cannot tell the difference between foreign substances and its cells and tissues. The immune system then makes antibodies directed against itself. These antibodies — called “auto-antibodies” (auto means ‘self’) — cause inflammation, pain, and damage in various parts of the body.
Unfortunately, there is no cure for lupus. Treatment can only hope to make the sufferer comfortable at best. It is for this reason that early detection is so important.
Types of Lupus
The most common type of lupus is SLE (systemic lupus erythematosus). It is a complex and baffling condition that can target any tissue or organ of the body. Common targets include: the skin, muscles, joints, blood and blood vessels, lungs, heart, kidneys, and the brain. For some people, only the skin and joints will be involved. In others, the joints, lungs, kidneys, blood, or other organs and/or tissues may be affected. Generally, no two people with systemic lupus will have identical symptoms.
There are other types of lupus that mainly affect the skin. Discoid lupus or Chronic cutaneous lupus erythematosus (CCLE) is always limited to the skin. It is identified by a rash that may appear on the face, neck, and scalp. Discoid lupus is diagnosed by examining a biopsy of the outbreak. In discoid lupus, the biopsy will show abnormalities that are not found in the skin without the rash.
A few individuals develop drug-induced lupus as a response to some medications used to treat other conditions. These symptoms disappear when the person stops taking the medication.
Neonatal lupus is a rare condition acquired from the passage of maternal autoantibodies, specifically anti-Ro/SSA or anti-La/SSB, which can affect the skin, heart, and blood of the fetus and newborn. It is associated with a rash that appears within the first several weeks of life and may persist for about six months before disappearing. Congenital heart block is much less common than the skin rash. Neonatal lupus is not systemic lupus.
General symptoms
- Each person’s experience will be different, and the diagnosis of lupus must be made by a doctor. Some people will have only a few of the many possible symptoms. Because it can target any of the body’s tissues, lupus is often challenging to identify or diagnose. That’s why it is called “the disease with 1000 faces”.
- Before symptoms specific to lupus occur, flu-like symptoms may appear, along with severe fatigue, a sudden unexplained loss or gain in weight, headaches, hair loss, hives, high blood pressure, or changes in the color of fingers in the cold.
- Any of the following may indicate to a doctor that lupus is present. However, many of these symptoms overlap with Arthritis diseases, so you need to see a rheumatologist for diagnosis. This list is a small sample of the signs that a person with lupus may experience:
- Joint pain, sometimes with swelling, redness, and heat
- A red rash across upper cheeks and bridge of the nose
- Extreme fatigue
- An unusual reaction to sunlight
- A red scaly rash
- Small, usually painless sores inside the nose or mouth
- Chest pain, worse when lying down or inhaling
- Swelling of feet and legs, weight gain
- Seizures or severe psychological symptoms
- Abnormalities in blood chemistry which show up in blood tests
Diagnosis
Because many lupus symptoms mimic other illnesses, are sometimes vague and may come and go, lupus can be challenging to diagnose. The physician usually makes the diagnosis after a careful review of a person’s entire medical history coupled, an analysis of the results obtained in routine laboratory tests, and some specialized tests related to immune status. Although there is no single test available, there are many laboratory tests that can aid the physician in making a lupus diagnosis.
Routine clinical tests which suggest that the person has an active systemic disease include: sedimentation rate (ESR) and CRP (C-reactive protein) binding, serum protein electrophoresis which may reveal increased gammaglobulin and decreased albumin, routine blood counts which may show anemia and low platelet and white cell counts, routine chemistry panels which may reveal kidney involvement by increases in serum blood urea nitrogen and creatinine abnormalities of liver function tests, and increased muscle enzymes (such as CPK) if muscle involvement is present. This is not a comprehensive list of tests, and any of these also help diagnose other non-lupus diseases. The task of identifying the condition is very complicated and can take some time to analyze and determine your specific diagnosis.
Treatment
Treatment is based on the specific needs and symptoms of each person. Because the characteristics and course of lupus may vary significantly among people. It is important to emphasize that a thorough medical evaluation and ongoing medical supervision are essential to ensure proper diagnosis and treatment.
Medications are often prescribed for patients, depending on which organ(s) are involved, and the severity of involvement. Effective patient-physician discussions regarding the choice of medication, its possible side effects, and any changes in doses are vital. Common medications include non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, corticosteroids, antimalarials, immunomodulating drugs, and anticoagulants.
Relaxation Techniques
Art Therapy for Stress Management
Youth with Lupus
May is Lupus Awareness Month. Stay informed about all events and updates .
